- 欢迎来到北京优尼康生物科技有限公司
- |
-
商品分类

 010-64814275
010-64814275

 010-64814275
010-64814275

ENGLISH INTENDED USE:
For in-vitro diagnostic use. Measurement of platelet aggregation.
SUMMARY AND EXPLANATION:
- Investigation of congenital (eg: Glanzmann’s thrombasthenia, gray platelet syndrome, storage pool disease,…) or acquired thrombopathy (eg: myelodisplasic or myeloproliferative syndrome, Waldenström’s disease, multiple myeloma,…).
- Follow-up of patients treated with antiplatelet drugs such as aspirin, thienopyridines, abciximab and other NSAIDs and GPIIbIIIa inhibitors.
ASSAY PRINCIPLE:
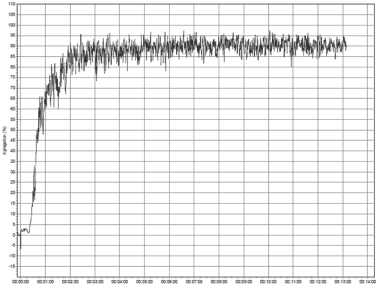
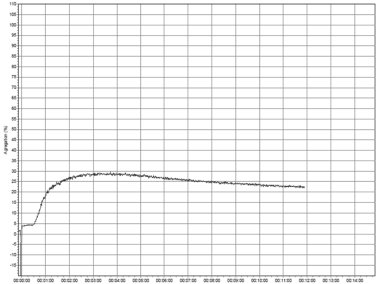
When added to platelet rich plasma (PRP), collagen adheres to platelets through receptors GPIa/IIa and GPVI. GPVI receptor is responsible for platelet activation leading to ADP and thromboxane A2 release, and calcium mobilization (1, 2, 3). Platelet aggregation in response to collagen typically displays a collagen concentration-dependent lag phase, then a platelet shape change, resulting in a transient decrease of light transmission, followed by a single wave of aggregation. Collagen is considered as a “strong” agonist.
REAGENT AND DILUENT:
- 3 vials of 0.5 mL of Collagen reagent, lyophilized in the presence of stabilizers. Product origin: collagen from equine tendon (mainly type I). The concentration of collagen is 1 mg/mL after reconstitution with 0.5 mL of distilled water.
- 3 vials of 12 mL of Collagen diluent.
REAGENTS AND MATERIAL REQUIRED, BUT NOT SUPPLIED:
SD Medical Platelet aggregometer (or equivalent), used as per manufacturer’s instructions, with suitable stirrers and aggregometer cuvettes.
Pipettes with variable dispensing volumes from 15 μL to 1,000 μL.
Fine and long pipette tips (for collagen injection).
Glass tubes.
Distilled water, preferentially sterile.
STORAGE CONDITIONS:
Reagents must be stored at 2-8°C, in their original packaging box. They are then stable until the expiration date printed on the box.
Note: Stability studies for 3 weeks at 30°C show that the reagents can be shipped at room temperature for a short period without damage.
REAGENT PREPARATION AND STABILITY:
Reconstitute each vial with exactly 0.5 mL of distilled water to get a solution at 1 mg/mL.
Shake thoroughly until complete dissolution of the content (vortex). Let to homogenize for 30 minutes at room temperature (18-25 °C), while shaking the vial from time to time.
Homogeneize the content before each use.
Restored Collagen Reagent and Collagen diluent after opening are stable as described below when kept in their original vials, protected from evaporation and contamination:
4 weeks at 2-8°C.
24 hours at room temperature (18-25 °C).
Do not freeze.
Cautions:
- As for any product of biological origin, handle with all the required cautions, as being potentially infectious.
- In order to improve stability, the reagent must be closed with its original screw cap following each use Reagents must be handled with care, in order to avoid any contamination during use.
- Incubating the reconstituted vial(s) for 30 min. at RT allows stabilizing the reagents, and obtaining a homogeneous reactivity.
- Take care to limit as much as possible any evaporation of the reagents during use.
- Vials are closed under vacuum. Remove carefully the stopper, in order to avoid any loss of powder when opening the vials.
SAMPLE COLLECTION AND PREPARATION:
In case of thrombopathy investigation, patients should be out of any medication known to affect platelet function (eg aspirin) for 10 days prior to specimen collection.
Patients should avoid fatty foods, coffee and dairy products for at least 12 hours prior to specimen collection.
Blood collection should be performed with care to avoid stasis, hemolysis, contamination by tissue fluids, or exposure to glass.
Blood (9 vol.) must be collected through a clean venipuncture on 0.109M (or 0.129M) trisodium citrate anticoagulant (1 vol.), taking care of completely filling the tubes. Cover and invert 4-5 times gently to mix; Maintain specimen at room temperature (18° to 25°C). Avoid blood collection using CTAD tubes.
Refer to GEHT or NCCLS/CLSI guidelines for further instructions on specimen collection, handling and storage.
Discard any unusual sample with an unusual aspect eg abnormal hematocrit, hemolysis, RBC contamination, lipemia, icterus, thrombocytopenia (<75,000/mm3), clots in specimen, and hypofbrinogenemia….which may interfere in the test and affect the results.
PREPARATION OF PLATELET RICH PLASMA (PRP) AND PLATELET POOR PLASMA (PPP):
1) Prepare PRP by centrifuging the citrated blood at 150xg for 10 minutes at room temperature (18°C to 25°C).
2) Examine the plasma layer for red cells. If red cells are present, re-centrifuge at 150xg for an additional 5 minutes.
3) Using a plastic transfer pipette, observe and carefully remove the platelet layer without disturbing the buffy coat or red cells, and transfer to a container labelled (PRP). Cap the container and allow it to stand at room temperature.
4) Prepare the PPP by centrifuging the remaining blood specimen at 2000-2500 x g for 15 minutes. Examine the PPP for hemolysis, then transfer it to a plastic tube labelled PPP. Cap the container and allow it to stand at room temperature.
5) The platelet count of the PRP should be 250,000 ± 50,000/mm3. The platelet count may be reduced by using PPP prepared from the sample.